Role of Regenerative Medicine in Orthopedics
At CalSpine MD, Dr. Ball’s goal is to provide the latest in minimally invasive therapies that will replace, repair, or promote tissue regeneration for acute and chronic orthopedic conditions as well as spinal pathologies using acellular amnion-derived allograft, platelet-rich plasma (PRP), and other methods that amplify the body’s natural biology to repair injured or damaged tissue. When used in correct concentrations and doses, these therapy options may help speed up the healing process of broken bones, injured muscles, tendons, and ligaments (musculoskeletal injuries) and discs in the spine.
Acellular Amnion-Derived Allograft
Benefits of Acellular Amnion-Derived Allograft
These products, made from substances that are naturally found in your body, help to improve the quality of healing, offering better and stronger tissue and less scar tissue. For athletes, they offer an alternative to steroid injections–they are joint preserving, reduce inflammation, and do not harm cartilage. Repeated cortisone or steroid injections to a joint cause ruptures of ligaments, cartilage damage, or nerve damage.
Platelet-Rich Plasma (PRP) Therapy
How It Works
The process begins with a sample of your blood. It is spun around in a centrifuge that separates platelets, plasma, and red and white blood cells. The platelets are then concentrated and mixed with some of the plasma. This mixture is called “platelet-rich plasma.” Dr. Ball injects this into the site of your injury. After the injection, your immune system (the system that keeps your body healthy) reacts quickly, and special white blood cells called “macrophages” rush in to take away damaged cells. Macrophages help prep the site for healing. Then, stem cells and other cells begin to multiply. Over time, they repair and rebuild the injured tissues.
Benefits of PRP Therapy
The Healing Process
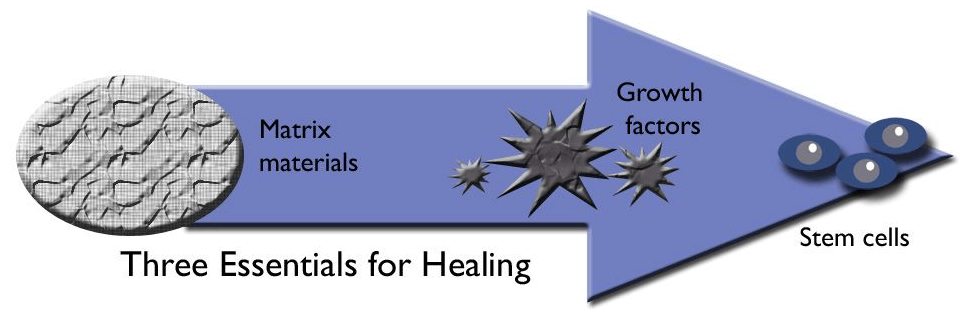
When you have a musculoskeletal injury, there is bleeding in the injured area. This bleeding is the foundation for the healing process, and it provides a way for healing factors to reach the injury site. These healing factors in combination with bleeding are all necessary for healing. Acellular amnion-derived allograft, regenerative extracellular matrix, and PRP may enhance the potency and speed of this healing process. They include matrix materials, growth factors, and stem cells.
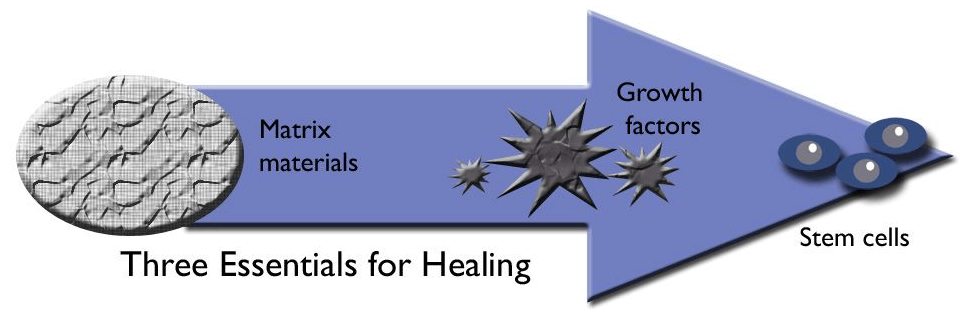
Matrix Material
Matrix material (or conductive material) provides housing or scaffolding for stem cells while they grow into mature cells. If stem cells do not have a house to grow in, they cannot develop into repair cells that can heal bone, muscle, tendon, or cartilage. These cells are also known as mesenchymal or undifferentiated cells.
When a patient breaks a bone, the healing process begins, and stem cells should be able to make new bone and promote healing. However, if a significant portion of the broken bone is lost due to a bone being fragmented, a large gap may result. In this instant, the gap must be filled with matrix to house stem cells. There are several substances that can be used to fill such gaps, during surgery including:
Bone Grafts. There are two types of bone grafts–an autograft and an allograft.
An autograft is a bone graft that is harvested from the patient, usually taken from the patient’s iliac crest, which is a part of the pelvis. Harvesting the bone graft requires an additional incision during the operation to treat the injury. This not only increases the time of surgery but it can also cause increased pain or risk of infection after the operation. Generally, patients have a good outcome; however, the harvesting site usually takes a while to heal.
An allograft is a bone graft that comes from cadaver bone supplied by a bone bank (bone tissue that is donated upon death). If the needed bone graft is available, this is the preferred method, as it avoids the risk of pain at the donor site. It does not heal as completely as bone from the same patient.
Artificial Matrix Material. Artificial matrix material, such as tricalcium phosphate or hydroxyapatite, can also be used to fill a large void between bone ends. It can form a material that closely resembles bone, and it contains holes that are the right size for stem cells to enter and develop into mature cells.
Growth Factors
Stem Cells
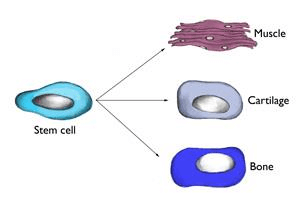
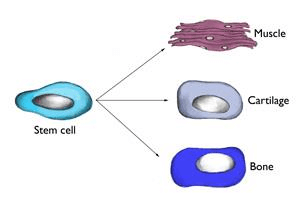
Stem cells are undifferentiated cells that are capable of giving rise to indefinitely more cells of any type. These immature cells can develop into many different cell types in the body and have the greatest potential for promoting healing, as they function as an internal repair system replenishing other cells where needed to promote healing. Each divided cell, therefore, has the potential to become another type of cell needed to help in healing–bone, muscle, ligament, and cartilage.
Stem Cells Speed Up The Healing Process
Stem Cell Therapy
Stem Cell Types
Misconceptions About MSCs
Justifying the Use of Stem Cells
Regenerative Medicine at CalSpine MD